Infectious Retinitis
Infectious retinitis is an inflammation of the retina resulting from infection by viruses, bacteria, fungi, or parasites. These pathogens affect patients differently depending on characteristics like age, location, and immune status. Treatment is aimed at preventing permanent vision loss and protecting the fellow eye.

Symptoms:
Some patients with infectious retinitis will notice “floaters” or decreased vision, while others have no symptoms at the time of diagnosis. Observed floaters in the gel of the eye may be collections of inflammatory cells, or cells released from retinal breaks or bleeding. Vision is blurred by inflammatory haze within the eye and by involvement of specific retinal areas that give central vision. Symptoms can appear suddenly or slowly progress.
Children with congenital infections, those whose mothers were actively infected during pregnancy or childbirth, may have misaligned eyes, involuntary eye movements, or an abnormal white reflex through the pupil (Figure 1).
Some patients are sensitive to light and have red, painful eyes, while others may be systemically ill, with symptoms including fevers, chills, and unintentional weight loss.
Causes:
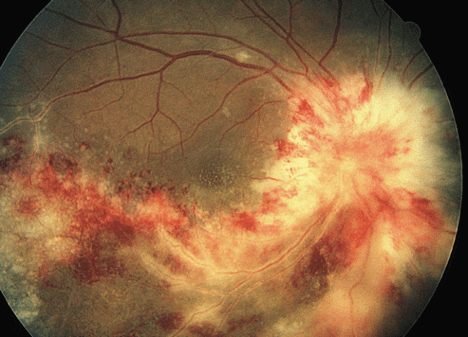
A variety of microbes cause retinitis. Herpes simplex virus (HSV) and herpes zoster virus (HZV) can lead to acute retinal necrosis (ARN) and progressive outer retinal necrosis (PORN). Cytomegalovirus (CMV) is in the same viral family and can cause retinitis in patients with compromised immune systems (Figure 2).
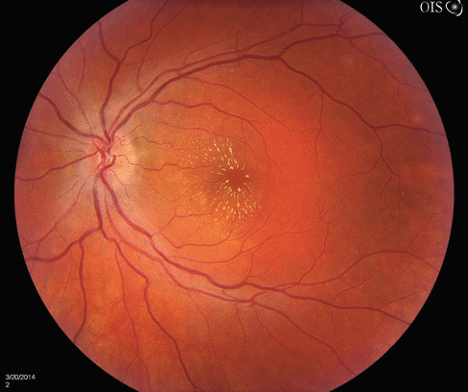
Retinitis also may be associated with cat-scratch disease from Bartonella species carried by cat fleas (Figure 3), with Lyme disease from Borrelia burgdorferi carried by Ixodes ticks, with syphilis caused by Treponema pallidum or tuberculosis caused by Mycobacterium species.
Some patients harbor infection else-where in their bodies, which eventually seeds the eye. These endogenous (caused by factors inside the body) intraocular infections may be bacterial, but may also be fungal, from yeasts like Candida species or molds like Aspergillus species. Some parasites also cause infectious diseases like toxoplasmosis, toxocariasis, and diffuse unilateral subacute neuroretinitis (DUSN).
Risk Factors:
Significant risk factors include active maternal infection during pregnancy or childbirth, exposure to endemic areas, or being immunocompromised. A compromised immune system may be weakened by medication, malignancy, or infection, as in the case of acquired immunodeficiency syndrome (AIDS). Immunosuppressive medications include antiinflammatory steroids, as well as drugs used to treat patients with cancer, autoimmune disease, and after organ transplantation.
Intraocular infections may develop in patients with infected heart valves, gastrointestinal tract infections, and urinary tract infections, as well as in those who use intravenous drugs or who take long-term antibiotics. In these endogenous infections, the infective agent is spread from another part of the body to the eye.
Diagnostic Testing:
To make a specific diagnosis, intraocular fluid samples may be taken and sent for analysis. In some cases, blood or cerebrospinal fluid (CSF) are also tested. Imaging may be done to help make the diagnosis.
Treatment and Prognosis:
Treatment is directed at the source of infection. In some cases, local therapy can be administered via injections into the eye, but oral or intravenous medications are sometimes necessary. Laser procedures or surgery are indicated for some infections.
Visual outcomes are variable depending on the specific sites of retinal involvement. For example, Toxoplasma infections are usually selflimited and can be observed, whereas herpetic viral infections are more serious and can lead to retinal detachment. Early diagnosis of infectious retinitis is crucial in trying to ensure the best visual outcomes.
Copyright 2016 The Foundation of the American Society of Retina Specialists. All rights reserved. savingvision.org I 20 North Wacker Drive, Suite 2030, Chicago, IL 60606 | (312) 578-8760

