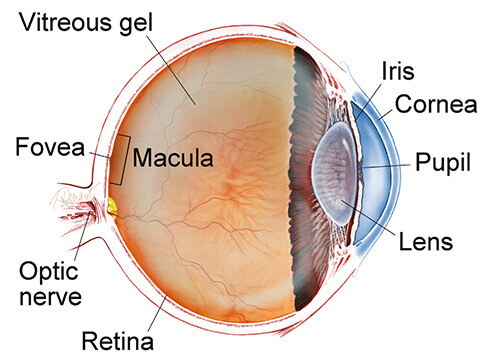
The many layers of the retina work together to convert light focused on the retina into an exquisitely detailed message that travels to the visual cortex in the brain. There, the message is decoded and directs us to take action — “that’s a fine looking piece of pie!”
The macula is the part of the retina that helps us see fine detail, faraway objects, and color. It’s packed with more photoreceptors (light-sensitive cells) than any TV or monitor. The small, central area of the retina is worth the most— the bullseye of sight. Macular edema, degeneration, hole, pucker, drusen (small yellowish deposits), scar, fibrosis, hemorrhage, and vitreomacular traction are common conditions that involve the macula. When macular disease is present, distorted vision (metamorphopsia), blank spots (scotoma), and blurred vision are common symptoms.
Symptoms and Causes:
Macular edema refers to an abnormal blister of fluid in the layers of the macula. From the side, it looks like the snake that ate too much. Like a droplet of water on your computer screen, the swollen retina distorts images— making it more difficult to see clearly. The more widespread, thicker, and severe the swelling becomes, the more likely one will notice visual symptoms of blur, distortion, and difficulty reading.
If untreated, chronic macular edema can lead to irreversible damage of the macula and permanent vision loss. Macular edema is typically caused by increased leakage from damaged retinal blood vessels or growth of abnormal blood vessels in the deep retina. New vessels (neovascularization or NV) do not have normal “tight junctions” and almost always result in abnormal leakage of fluid (serum from the bloodstream) into the retina.
Diagnostic Testing:
Fluorescein angiography (Figure 1) and optical coherence tomography (OCT; Figure 2) are 2 common tests to evaluate macular edema. Based on the appearance of fluid on these tests, macular edema may be widespread, localized, or be made up of many small blisters surrounding the center of the macula—a common form called cystoid macular edema.

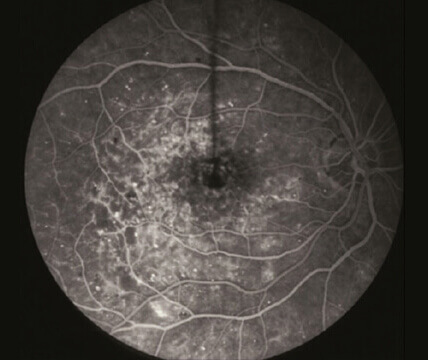
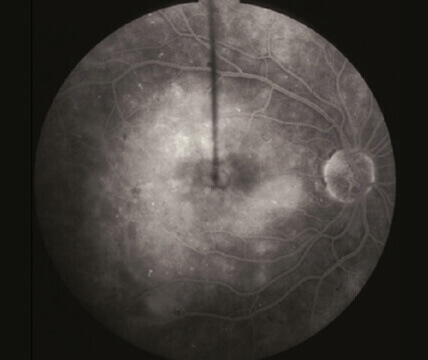
Figure 1
Fluorescein angiography in the left eye of a patient with severe changes of diabetic retinopathy. The numerous small white spots represent weak, dilated areas of the retinal blood vessels, called microaneurysms. These are well seen in the early phases of the angiogram (above). In the right eye of a different patient, the pinpoint microaneurysms (above center) become fuzzy in appearance as the fluorescein dye leaks from the blood vessels into the surrounding retinal tissue (above right). When leakage involves the central retina, it is called macular edema.
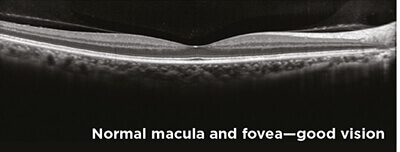
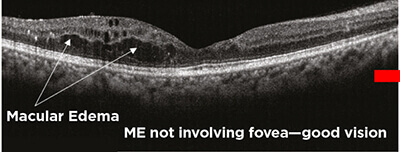
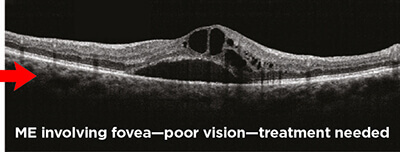
Figure 2
Optical Coherence Tomography and Macular Edema (Images courtesy of the ASRS Retina Image Bank, contributed by Dr. Suber Huang) OCT is a useful test to study macular edema (ME).
- The top image is normal. Note the even layers and gently sloping dip of the macula called the fovea. This eye has excellent vision.
- The middle OCT has ME, black-appearing cysts (arrows) which threaten the normal fovea. This eye also has good vision.
- The bottom OCT shows ME involving the macula. Because ME involves the macular center (the fovea), vision is poor (large red arrow).
Treatment and Prognosis:
The most effective treatment strategies for macular edema address the underlying cause (diabetes, blood vessel occlusion, neovascularization, inflammation, etc), as well as an excess of fluid leaking from abnormal blood vessels in and around the macula. Eye drops, laser, and surgery can be effective in many diseases, but the mainstay of treatment is intravitreal injections (IVI).
The IVI is an office procedure performed under topical anesthesia in which medication is placed inside the eye by a very small needle. The injection generally causes little to no pain. IVI should be performed by a trained retina specialist with meticulous monitoring of treatment efficacy and detection of rare but potentially serious complications. IVI is now considered one of the most commonly performed medical procedures.
Ranibizumab (Lucentis®), aflibercept (Eylea®), and dexamethasone (Ozurdex®) are the generic and trade names, respectively, of the 3 most widely used FDA-approved medications for IVI treatment of the common conditions causing macular edema. Bevacizumab (Avastin®) is not FDA approved for this use, but has also been extensively studied in large, well-designed, federally funded clinical trials and is felt to have excellent efficacy. US physicians are permitted to use drugs in a manner not included in the FDA’s approved packaging label; this common practice is known as off-label use.
Each treatment option has a considerable track record of success and works by decreasing the amount of fluid leaking from abnormal blood vessels. There are differences between each of these drugs. Your retina specialist will work with you to identify which options are best for you.
Macular edema is a common finding in many diseases of the retina, almost all of which can be treated to improve vision. As with other conditions, the visual prognosis depends on the severity of the underlying condition, its duration, the general health of the eye, and the degree to which vision has been affected.
There has never been a more successful time in the treatment of macular edema from a variety of causes, and more promising therapies will be available in the future.
Copyright 2016 The Foundation of the American Society of Retina Specialists. All rights reserved. savingvision.org I 20 North Wacker Drive, Suite 2030, Chicago, IL 60606 | (312) 578-8760

